Cancers of the Eyelid | Skin Cancers around the Eye
Eyelid cancer work forms a significant proportion of work for most oculoplastic surgeons. The management of most eyelid cancers involves surgery to remove the cancer followed by reconstruction of the region to give as good a functional and cosmetic result as possible for the patient.
All skin cancers around the eyelids are designated as high risk skin cancers by the British Association of Dermatologists and as such should be treated seriously.
Basal Cell Carcinoma
Basal cell carcinoma (rodent ulcer) is the commonest cancer of the eyelid. The classic presentation of a BCC is a hard nodule with a pearly edge, often with dilated blood vessels on its surface (telangiectasia) and central ulcer formation as the BCC enlarges.
Eyelid BCCs arise from within the superficial layers of skin, most commonly involving the lower eyelid. The risk of BCC development in any particular person is related in part to the fairness of that person’s skin and the amount of sun exposure that person receives. Although it does not spread to distant sites (metastasis), it can continue to enlarge and invade surrounding structures. On the whole, surgery for larger tumours is likely to be more extensive.
Although the best chance of cure of eyelid cancers is via complete surgical removal; some patients with BCC may be treated with other methods e.g. radiotherapy, cryotherapy, topical chemotherapy, immunotherapy.
Less commonly, other types of cancers may develop around the eye e.g. malignant melanoma, squamous cell carcinoma, sebaceous gland carcinoma. They are by far much less common than BCCs, but their management on the whole requires more radical treatment than BCCs, at times involving joint care with other types of doctors e.g. oncologists, maxillofacial surgeons, general plastic surgeons, due to their ability to spread to distant sites.
BCCs differ from most cancers in that they rarely spread to distant sites.
Eyelid Cancer Surgery Gallery
Click images to start gallery
(Warning: some of the pictures are quite graphic and may cause distress)
-
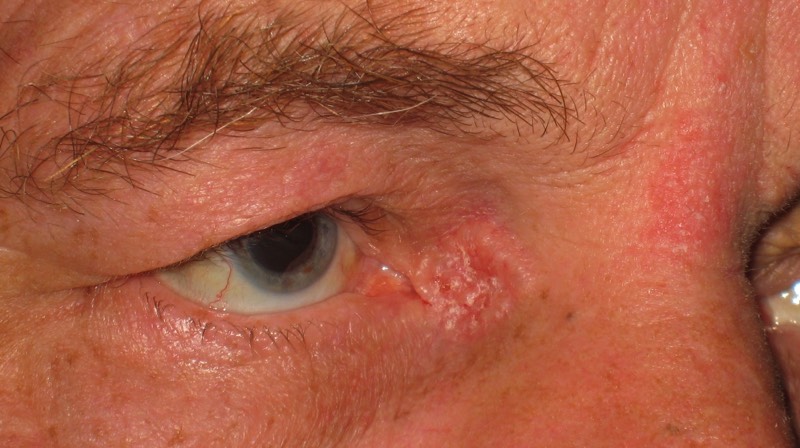
This skin cancer had been slowly growing for 6 months
-

Resultant defect in eyelid after surgery to remove the cancer first
-

The defect has been reconstructed with a hughes flap.
-

The Hughes flap is allowed to heal for 2 weeks meaning the patient cannot open her affected eye.
-

After 2 weeks, the Hughes flap is opened with surgery. The patient can open her eyelids normally and is pleased with the cosmetic result.
-

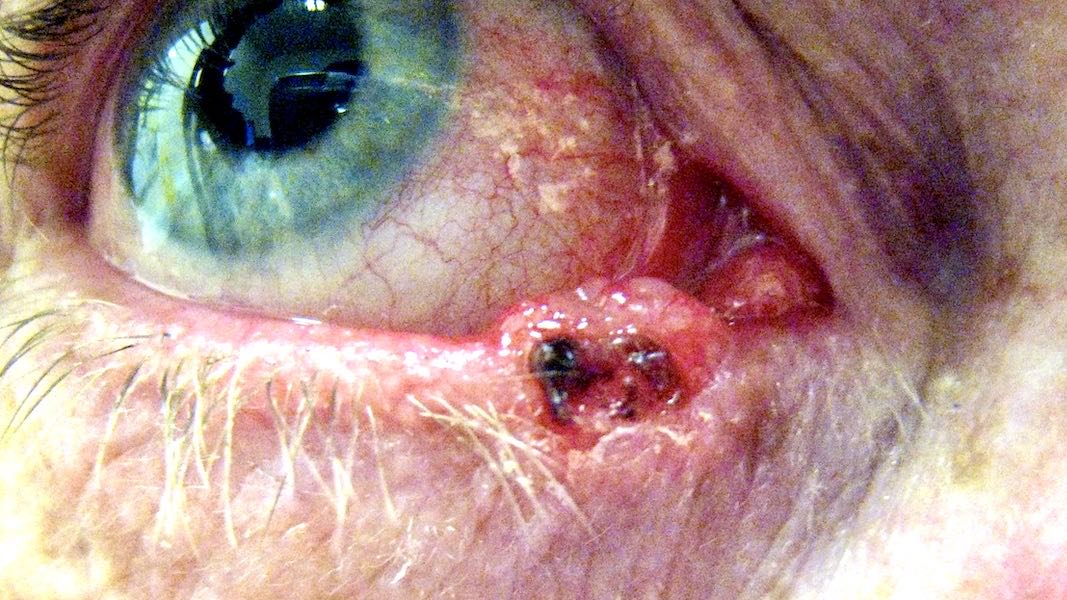
This skin cancer had been slowly growing for 2 years
-

The skin cancer has been marked ready for surgical removal. Note cancer is removed with a rim of normal skin to ensure complete removal of the skin cancer.
-

The resultant skin defect following removal of the skin cancer. This defect is going to be closed using a large sliding skin flap.
-

2 weeks following reconstruction with skin flap. Notice the flap is still thickened. The patient is asked to massage the flap with antiscarring silicone gel for 3 months following surgery.
-

4 months following surgery. The flap has become invisible. The patient is very happy with the cosmetic and functional result.