Thyroid Eye Disease
What is Thyroid Eye Disease?
Severe thyroid eye disease: The eyeballs become can become very exposed leading to symptoms of ocular dryness.
In the UK, thyroid eye disease is the most commonest cause of inflammation affecting the eye socket.
Thyroid eye disease (sometimes abbreviated as TED) is an uncommon condition affecting patients who suffer from problems related to the thyroid gland.
The most common thyroid disorder associated with TED is Graves’ Disease and roughly 40% of patients with Graves’ disease will go on to develop TED.
The most common abnormalities experience by TED sufferers are prominent poppy bulging eyes, a staring expression and the sensation of the eyes feeling dry.
What causes Thyroid Eye Disease?
Hyperthyroidism is a condition in which there is overproduction of thyroid hormones. It is thought to occur as part of an autoimmune disorder, where the patient’s own immune system starts to attack the thyroid gland causing it to become overactive. In a similar way, the immune system also produces abnormal antibodies which attack some of the soft tissue structures around the eye itself e.g. tendons, muscles and fat, resulting in their swelling and scarring. As a result, these soft tissue structures start to change. For example, the extraocular muscles, which control the position of gaze of the eye itself, can start to swell. Eye movements become sore, the eyes feel warmer to touch, double vision may result and the eye may start to protrude forward out of the bony socket (proptosis).
Clinical Features of Thyroid Eye Disease?
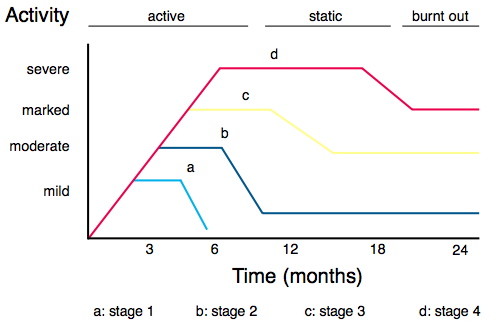
The Rundle Curve: This describes the stereotypical disease paths of patients with TED.
Most patients start to notice eye problems at the same time as the onset of their thyroid problem. For some patients, thyroid eye disease may develop some years either before or after the onset of the actual hormone imbalance. When TED starts to become apparent, most patients are hyperthyroid, with a smaller proportion euthyroid (normal thyroid activity) or hypothyroid (underactive thyroid activity).
Both eyes are usually affected, although the severity of disease may differ dramatically between left and right. Classically, TED is described to go through different cycles, with an active phase (characterised by orbital inflammation), a static phase (characterised by no change in activity) and burnt out phase (when there is no longer any signs of activity) with patient’s symptoms and signs reflecting the current phase. How long each phase lasts and the severity of each phase varies from patient to patient.
During the active phase, patients often notice the sensation of pressure around the eyes with irritation, redness and tearing. Inflammation of the structures around the eye also causes the same structures to become scarred. Inflammation of the fat and muscles around the eye cause their enlargement, resulting in the eye being pushed forward and the sensation of pain in different positions of gaze as the muscles become stretched. If the muscles become too swollen, the enlarged muscles can compress the optic nerve (the main nerve which takes information from the eye to the brain) resulting in blurring/ loss of vision.
After several months, as the active inflammation starts to wear off (static phase), the patient’s eyes feel less wet and inflamed. Eventually the inflammation disappears completely and the previously engorged swollen soft tissues start to shrink back to normal size (burnt out phase). However, any scarring, which developed when the TED was active, remains. Scarring of any structure means that it becomes less able to stretch.
For example, the muscles which control the position of the gaze of the eye may have become scarred, leading to double vision.
Similarly, scarring of main tendon involved in controlling the movement the upper lid, may result in an inability for the upper lid to descend properly, resulting in a staring appearance (upper lid retraction). Sometimes this may be so severe that the cornea may become dry from overexposure.
Many patients will be left with some degree of protrusion of the eye itself, lid retraction, or double vision that may require additional treatment.
Is Thyroid Eye Disease Dangerous?
Thyroid eye disease if severe enough can threaten sight. Increased exposure of the cornea from eyeball protrusion or lid retraction can lead to corneal scarring. Double vision can be severe and disabling. If the swelling is severe enough, the pressure in the orbit (eye socket) can become extremely high and compress the optic nerve. The person may experience progressive loss of vision, and possibly blindness if the condition is not treated promptly. However, it must be stressed that most patients with TED suffer only a mild short lived form. Only a small proportion of patients develop the severe, sight threatening type.
Thyroid Eye Disease Treatment
All patients with significant TED should be under the care of an ophthalmologist who is able to monitor them regularly. Ideally, the ophthalmologist should be able to work closely with the the patient’s GP/ endocrinologist.
The principles behind the treatment of TED involve:
Ensuring that the patient is euthyroid and stopping/ refraining from smoking
It is vital that all patients ensure that they do not smoke and that their thyroid hormones are as well controlled as possible.
Selenium
There is now strong evidence to suggest that patients with thyroid eye disease taking selenium supplements during the initial active phases of their disease will develop less severe long term changes and have a shorter active disease phase.
Reducing exposure symptoms
For the vase majority of TED sufferers who suffer from mild symptoms of overexposure of the eyes only, the use of eye drops, wrap-around tinted glasses, sleeping with eye shield with the head elevated can have a dramatic effect.
Reducing the effects of inflammation in patients in their active phase
When there is active inflammation with more severe symptoms, oral steroids or other anti-inflammatory medications may be needed to reduce the swelling. Radiation treatment is sometimes used to treat active inflammation as well.
Treating sight threatening emergencies
In patients with sight threatening complications emergency surgery may be necessary to preserve vision. For example, severe overexposure of the cornea may lead to ulcer formation unless treated by orbital decompression surgery (removing part of the bony orbit and/or fat behind the eye) to restore the position of the eyeball back into the socket or by improving the closure of the lids with lid surgery. Unless sight threatening emergencies develop, most surgeons aim to perform rehabilitative surgery during the burnt out phase of the disease.
Cosmetic and functional rehabilitation
The function and appearance of the eyes can usually be improved by surgery. Each type of operation will carry with it its own set of risks and benefits; thus patients can opt different types of surgery depending on the severity of their eye problems, their expectations for improvement and his/her attitude to the risk.
For example. many patients do opt for orbital decompression since it often has dramatic results improving coverage of the eyes themselves, allowing their eyes to return back to their normal position within the socket thus reducing the bulging/ staring appearance of the eyes. However some patients decline decompression surgery because of the small risk of blindness.
Misalignment of the eyes and double vision can be improved with eye muscle surgery (squint surgery) or optical prisms.
Eyelid surgery (lid elevation or lowering) to adjust the position of retracted lids can improve eyelid closure and restore eyelid function.
Removal of excessive fat and skin (blepharoplasty) from the eyelids can also improve their appearance.
Is the surgery effective?
While it may not be possible to completely eliminate all of the consequences of thyroid eye disease, surgery to correct these conditions is generally successful in satisfactorily restoring function, comfort, and cosmetic appearance.




